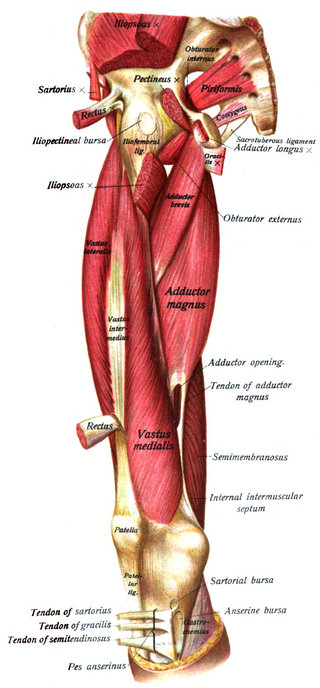
All Lower Quarter

One Leg, Eyes Closed, Arms Crossed, Head Tilt, and Rotation
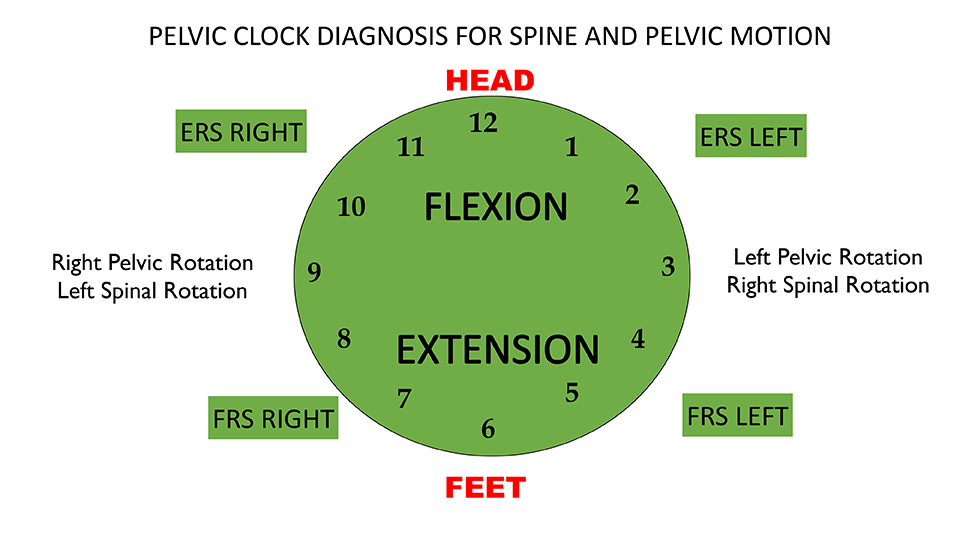
in 1 Sensorimotor Imbalances, 2 Movement Tests Lower Quarter, 5 Home Exercise Strategy, Active Trunk Rotation, All Home Exercises, All Lower Quarter, All Sensorimotor Imbalances, Hip ABD Firing Pattern, Hip EXT Firing Pattern, Pelvic Clocks, Rolling, Sensorimotor, Supine Curl Up, Supine Heel slide, Supine Hip ABD and ER